- Branch Retinal Vein Occlusion
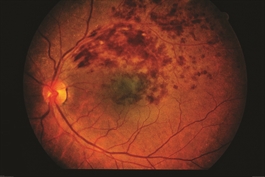
- Central Retinal Vein Occlusion
- Central Serous Chorioretinopathy
- Diabetic Retinopathy
- Epiretinal Membrane
- Lattice Degeneration
- Macular Hole
- Posterior Vitreous Detachment
- Retained Lens Fragments
- Retinal Artery Occlusion
- Retinal Detachment
- Retinal Tears
- Vitreomacular Traction

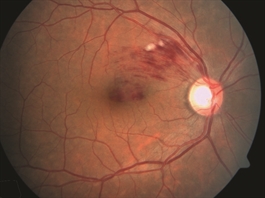
Branch Retinal Vein Occlusion
Symptoms
- Quick diagnosis
- Complex medical tests
- Early identification and intervention
- Complex surgical interventions
Causes
Most BRVOs occur at an arteriovenous crossing—an intersection between a retinal artery and vein. These vessels share a common sheath (connective tissue), so when the artery loses flexibility, as with atherosclerosis (hardening of the arteries), the vein is compressed.
The narrowed vein experiences turbulent blood flow that promotes clotting, leading to a blockage or occlusion. This obstruction blocks blood drainage and may lead to fluid leakage in the center of vision (macular edema) and ischemia—poor perfusion (flow) in the blood vessels supplying the macula.
Risk factors
- Uncontrolled high blood pressure
- Being overweight or obese (increased body mass index)
- Cardiovascular (heart) disease
- Glaucoma
- In younger patients who suffer BRVO, an abnormal tendency to develop blood clotting is also possible
Diagnostic testing
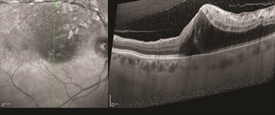
- Fluorescein angiography (FA)
- Optical coherence tomography (OCT)
- Venous stasis (congestion and slowing of circulation)
- Edema (swelling with fluid)
- Ischemia (inadequate blood supply) or
- Retinal neovascularization (abnormal growth of new blood vessels in the retina)
FA is very valuable for detecting BRVO and the flow of the blood vessels. Once BRVO has been found, OCT is used to provide a better assessment of whether macular edema is present, and if so, how severe it is.
Treatment and Prognosis
- Blood pressure monitoring
- Determining if blood cholesterol or lipid levels are elevated
- Blood tests, if appropriate, to determine if there is an abnormal tendency to form blood clots
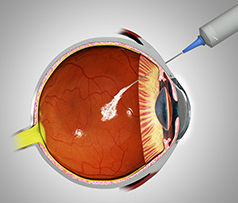
There are currently 3 anti-VEGF drugs:
- Avastin® (bevacizumab®)
- Lucentis® (ranibizumab®)
- Eylea® (aflibercept®)
Laser treatment may be used along with anti-VEGF therapy in hard-to-treat cases. Laser therapy for macular edema involves applying light laser pulses to the macula in a grid pattern. In a large multi-center clinical trial, after 3 years of follow up, this treatment showed improvement of vision in approximately two-thirds of patients.
Intraocular injections of steroids are another potential treatment for eyes that don’t respond to anti-VEGF drugs. A clinical trial that evaluated steroid treatment using a slow-releasing steroid implanted in the eye (dexamethasone or Ozurdex®), showed that approximately 30% of BRVO patients enjoyed significant visual improvement following treatment.
While intraocular steroids can have some side effects such as an increase in eye pressure and cataract progression, in most cases, these side effects can be controlled.
Overall, BRVO carries a generally good prognosis. In fact, some BRVO patients don’t require treatment at all, either because the blockage did not involve the macula, or because they have not experienced a decrease in vision. Over 60% of patients, treated and untreated, maintain vision better than 20/40 after 1 year.
Complications
When neovascularization develops, scatter laser photocoagulation therapy is used to create burns in the area of the vein occlusion (blockage). The aim is to try to lower the oxygen demand of the retina and thus stop the abnormal blood vessels from growing. Patients receive an anesthetic to numb the eye and make the treatment more comfortable.
Scatter photocoagulation has been shown to reduce neovascularization-related complications from 60% to 30%. Because only a few patients develop abnormal new blood vessels in the retina, not many need scatter photocoagulation treatment.
Retinal neovascularization is a potentially serious complication of BRVO in which an inadequate blood supply (ischemia) causes abnormal new blood vessels to grow on the surface of the retina. This growth can further decrease vision by causing vitreous hemorrhage that causes floaters and loss of vision, retinal detachment, and glaucoma.
When neovascularization develops, scatter laser photocoagulation therapy is used to create burns in the area of the vein occlusion (blockage). The aim is to try to lower the oxygen demand of the retina and thus stop the abnormal blood vessels from growing. Patients receive an anesthetic to numb the eye and make the treatment more comfortable.
Scatter photocoagulation has been shown to reduce neovascularization-related complications from 60% to 30%. Because only a few patients develop abnormal new blood vessels in the retina, not many need scatter photocoagulation treatment.
Eye Procedures
- Avastin® (bevacizumab®)
- Lucentis® (ranibizumab®)
- Eylea® (aflibercept®)

Lasik Eye Surgery
- At vero eos et accusamus et iusto odio
- But I must explain to you how all this
- praising pain was born and I will
Contact Info
San Diego
7695 Cardinal Court, Suite 100 San Diego, CA 92123
Office: (858) 609-7100
Fax: (858) 609-7106
info@sdretina.com
Oceanside
3231 Waring Court, Suite S, Oceanside, CA 92056
Office: (760) 631-6144
Fax: (760) 724-3920
info@sdretina.com
Locations
San Diego
Oceanside
Get In Touch