- Branch Retinal Vein Occlusion
- Central Retinal Vein Occlusion
- Central Serous Chorioretinopathy
- Diabetic Retinopathy
- Epiretinal Membrane
- Lattice Degeneration
- Macular Hole
- Posterior Vitreous Detachment
- Retained Lens Fragments
- Retinal Artery Occlusion
- Retinal Detachment
- Retinal Tears
- Vitreomacular Traction

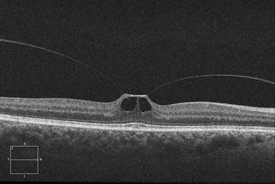
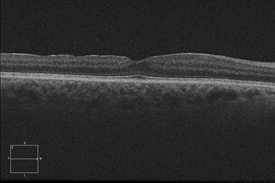
Vitreomacular Traction
There are instances where a PVD is incomplete, leaving the vitreous partially attached to the retina, and causing tractional (pulling) forces that can cause anatomical damage. The resulting condition is called vitreomacular traction (VMT) syndrome.
Symptoms
The most common symptoms experienced by patients with VMT syndrome are:
- Decreased sharpness of vision
- Photopsia, when a person sees flashes of light in the eye
- Micropsia, when objects appear smaller than their actual size
- Metamorphopsia, when vision is distorted to make a grid of straight lines appear wavy or blank
Causes
Weakening of the attachments of the vitreous cortex and the internal limiting membrane (ILM) of the retina could also lead to partial detachment of the posterior hyaloid membrane, leading to PVD and potentially VMT.
Risk factors
Other risk factors include:
- High myopia (extreme nearsightedness)
- Exudative (wet) age-related macular degeneration
- Diabetic macular edema
- Retinal vein occlusion
- Diabetic retinopathy
Diagnostic testing
A dynamic B-scan ultrasound examination could also be performed to provide a detailed evaluation of the vitreoretinal interface.
Treatment and Prognosis
- Watchful waiting and regular monitoring with OCT is often used for patients whose symptoms do not warrant active intervention. Some cases of VMT may spontaneously resolve.
- For patients whose symptoms are severe enough to require intervention, pars plana vitrectomy surgery is one treatment option. The procedure involves the manual release of vitreous attachment and alleviation of traction, but it is invasive and inconvenient to most patients. Therefore vitrectomy is reserved for patients who are at risk for severe visual disturbances and/or central blindness. Some studies have shown that shorter duration of symptoms results in better prognosis when the surgical treatment is employed.
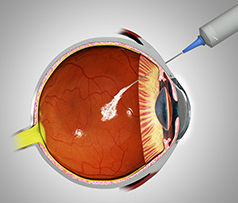
- Ocriplasmin (Jetrea®), a recombinant truncated form of human plasmin, is a pharmacologic option for treating VMT syndrome. Clinical trials demonstrated the efficacy and safety of a single intravitreal injection of ocriplasmin for the treatment of patients with symptomatic vitreomacular adhesion, and/or vitreomacular traction. Ocriplasmin is therefore a treatment option for some patients who have vitreomacular traction but who are not candidates for surgery.
- Pneumatic vitreolysis - a small gas bubble is injected into the eye in the office. Afterward, the patient will look down several times per hour for a day or two to try to get the gas bubble to sever the adhesion between the vitreous and the macula.
Retinal neovascularization is a potentially serious complication of BRVO in which an inadequate blood supply (ischemia) causes abnormal new blood vessels to grow on the surface of the retina. This growth can further decrease vision by causing vitreous hemorrhage that causes floaters and loss of vision, retinal detachment, and glaucoma.
When neovascularization develops, scatter laser photocoagulation therapy is used to create burns in the area of the vein occlusion (blockage). The aim is to try to lower the oxygen demand of the retina and thus stop the abnormal blood vessels from growing. Patients receive an anesthetic to numb the eye and make the treatment more comfortable.
Scatter photocoagulation has been shown to reduce neovascularization-related complications from 60% to 30%. Because only a few patients develop abnormal new blood vessels in the retina, not many need scatter photocoagulation treatment.
Eye Procedures
- Avastin® (bevacizumab®)
- Lucentis® (ranibizumab®)
- Eylea® (aflibercept®)

Lasik Eye Surgery
- At vero eos et accusamus et iusto odio
- But I must explain to you how all this
- praising pain was born and I will
Contact Info
San Diego
7695 Cardinal Court, Suite 100 San Diego, CA 92123
Office: (858) 609-7100
Fax: (858) 609-7106
info@sdretina.com
Oceanside
3231 Waring Court, Suite S, Oceanside, CA 92056
Office: (760) 631-6144
Fax: (760) 724-3920
info@sdretina.com
Locations
San Diego
Oceanside
Get In Touch